This didn’t come out of nowhere. After season one, episode two of chemo, I finally got back into the ocean. I’d been craving it since May. Cancer had hit pause on everything. Guincho was firing on the north side—rising tide, closer to high than low. I was cooked, caught a wave all the way in, felt great—right up until the wave drove me straight into the sand.
Immediate pain. Clavicle. Shoulder.
A specialist later called it a small fracture. The real problem wasn’t the injury itself; it was the timing. There was no real chance for healing while I was pumping chemotherapy into my body every other week. During chemo, the pain faded into the background. Adrenaline carried me. Then chemo stopped, and my body finally said, okay, now we recover. Every unresolved injury from the last couple of years started talking again. The clavicle didn’t whisper. It screamed.
Anti-inflammatories helped. The pain settled. Range of motion improved. Then chemo restarted—and the pain came roaring back with it.
Up to this point, imaging has been consistent. PET, CT, and MRI have all pointed to the same place: the left sternoclavicular joint, where the collarbone meets the sternum. Increased metabolic activity. Structural changes in the joint and nearby bone.
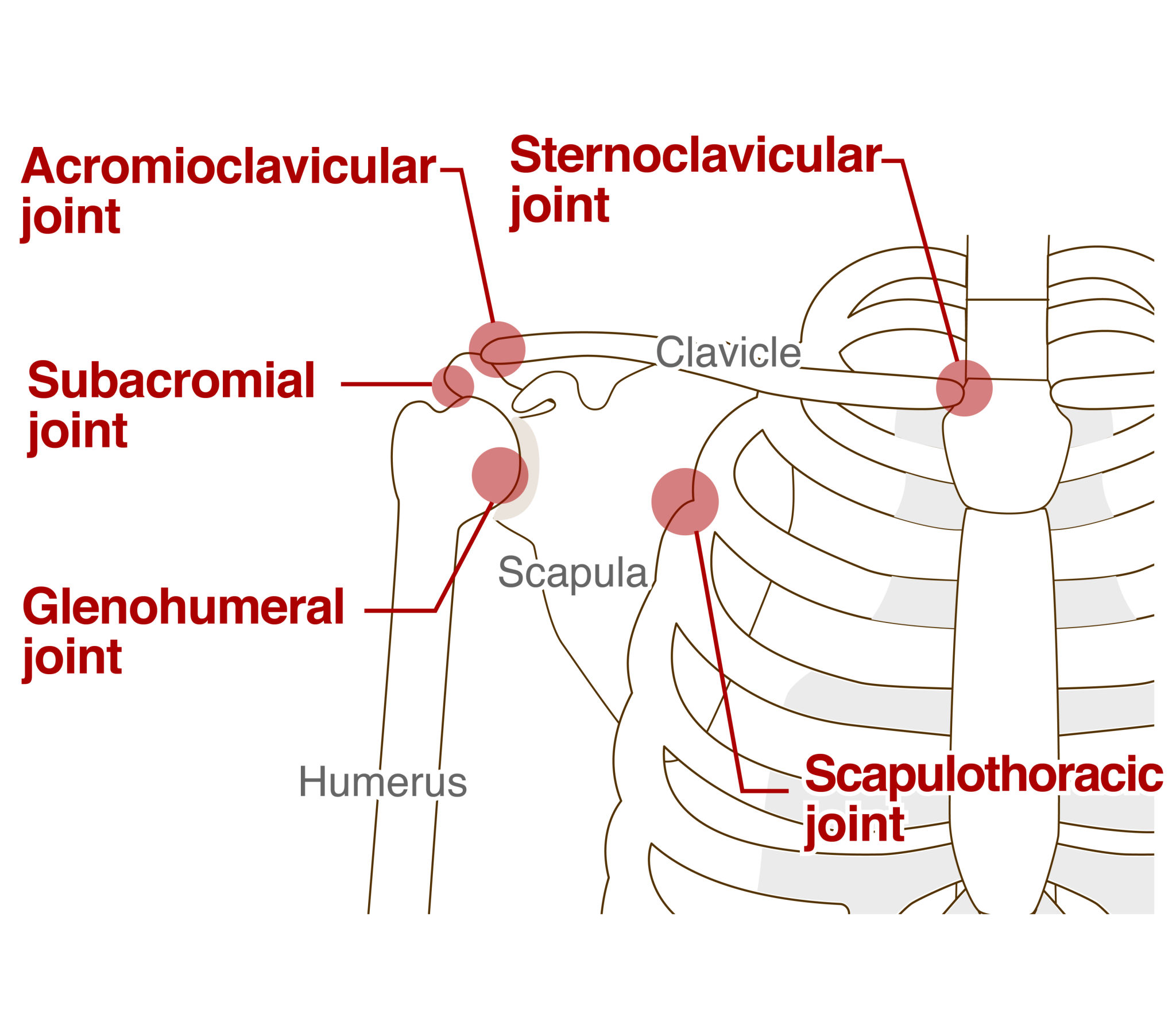
The pain is episodic. Some days, lifting my arm triggers sharp, limiting pain. Other days I’m back to maybe 60–70% mobility. It gets worse when I lie down too much. My neck, upper back, and shoulders tighten and lock everything in place. Movement helps. Rest makes it worse. That pattern fits inflammatory joint pain layered with muscle guarding.
Chemo complicates everything. It drives systemic inflammation, slows tissue repair, and stresses my liver enough that pain-control options are limited. The result is an inflamed joint that never fully settles, surrounded by muscles that clamp down to protect it. A feedback loop: pain, stiffness, reduced movement, more pain.
Muscle loss, restricted movement, and chronic pain don’t just hurt—they weaken the foundation. Rest is not recovery. Rest is reduced movement. If I want to keep momentum, this needs a clear plan.
I talked with my oncologist today.
Today’s appointment added both reassurance and urgency. My oncologist is happy that my creatine kinase levels are back to normal. That part worked. But she shares my concern about the amount of pain I’m dealing with.
I asked the question directly: have we fully ruled out bone metastasis? She didn’t dismiss it. Instead, she agreed that it needs to be definitively excluded. A PET scan has been ordered for this week, and chemo has been postponed one more week until we have clearer answers.
Pain options to discuss after the PET scan results:
• Continued topical NSAIDs
• Considering an image-guided corticosteroid injection directly into the sternoclavicular joint
• Referral to proper pain management (physiatry or interventional pain medicine)
• Physical therapy that understands sternoclavicular joint pathology—not generic shoulder rehab
 raig daniels
raig daniels